Telehealth Providers: How to Choose and What to Expect
What quality telehealth care looks like
Legitimate platforms make it clear that a prescription is not guaranteed. You’ll complete a detailed medical intake and meet a clinician licensed in your state by video or secure messaging. They will review your conditions, medications, and contraindications; discuss risks, benefits, and alternatives; set a titration plan; and schedule follow‑up to check side effects and progress. Prescriptions are sent to a state‑licensed U.S. pharmacy with transparent dispensing information (brand, strength, pen device, storage, refills). If labs or in‑person exams are clinically appropriate, they’ll order them or coordinate with your primary care team.
How the prescription is filled
Ask which pharmacy will dispense your medication and how it ships. For GLP‑1s, you should typically receive pre‑filled pens of an FDA‑approved product with standard patient labeling. Avoid services that ship unmarked vials requiring you to self‑measure doses, products referencing salt forms (e.g., “semaglutide sodium/acetate”), or items labeled “not for human use/research only.” Always verify the pharmacy’s license with your state board of pharmacy.
Common red flags
“Instant approval,” no clinician encounter, cash‑only bundles that include a “compounded GLP‑1,” social‑media DMs as the primary sales channel, overseas shipping, refusal to name the dispensing pharmacy, or instructions to mix or measure your own doses. Hidden ownership, no physical address, and vague refund policies are additional warning signs.
Questions to ask before you pay
- Are your clinicians licensed in my state, and will I meet one before any prescription?
- Which FDA‑approved GLP‑1 products do you prescribe, and when (if ever) do you use compounded versions? Under what specific medical criteria?
- Which pharmacy fills the prescription? Can you send it to a pharmacy of my choice?
- What does follow‑up look like (timing, messaging, emergencies)? Who do I contact for severe side effects?
- How do you handle prior authorization and appeals with my health plan?
- What are the total costs (visit, medication, shipping, membership), and are there cancellation or auto‑renewal terms?
- How do you protect my privacy and health data? Do you sell data to third parties?
If compounding is proposed
Compounding should be rare and tied to a documented, individualized medical need that a specific FDA‑approved product cannot meet (for example, a true excipient allergy). Confirm the clinical rationale in writing; ensure the pharmacy is state‑licensed (or a registered outsourcing facility); and confirm that the product does not use salt forms or “research‑only” materials. Request clear titration instructions, and keep all documents (labels, lot numbers, receipts) in case you need to report an adverse event.
Coordinate care
Ask the telehealth team to share your plan, dosing schedule, and any lab results with your primary care clinician or specialist. Integrated care helps catch side effects early and supports safe, sustained weight‑management.
Key Finding From Partner Research
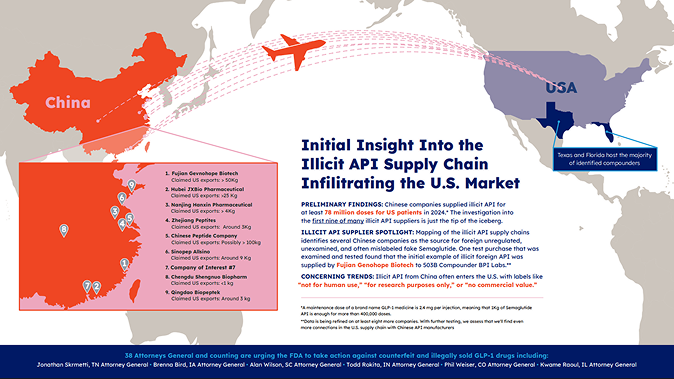
Illicit GLP‑1 Supply Chain — What we’re seeing
Partner research traces a pattern in which active pharmaceutical ingredients (APIs) for GLP‑1s are sourced from multiple overseas manufacturers, routed through intermediaries, and sold to U.S. compounders and gray‑market vendors. Some shipments are labeled “research use only/not for human use,” yet end up in products marketed to patients. At the point of sale, these products often appear as multi‑dose vials that require self‑measured dosing, are missing standardized patient labeling, and may lack consistent identifiers (e.g., lot numbers, NDCs, or clear expiration dates). This pathway increases the risk of poor quality, contamination, and dosing errors.
Additives found in illicit APIs — why they’re dangerous
Field reviews have identified unauthorized additives in certain illicit or non‑approved GLP‑1 materials. Examples reported include additional peptides (e.g., BPC‑157) and mixtures of vitamins/amino acids. Additives like these can change how the drug behaves in the body, create stability problems, and raise the risk of immunogenicity or other unexpected side effects. Because these formulations are not FDA‑approved, there is no assurance of purity, potency, or compatibility.